I’ve always been wary of fortune tellers and the last few years have been anything but predictable.
At the same time, navigating a start-up without a forecast is risky. Digital health is predicated on a futurist mentality, a passion for what is possible married with a careful study of the trends. In 2022, many longstanding trend lines bent sharply — diminishing some possibilities while enabling others.
Over the year this newsletter has documented many of the inciting events: the end of Roe and the fight for reproductive justice, the fierce industry sprints to address fertility and menopause, the promise and the peril of value-based care. In academia, a “preprint” is a time-critical version of scientific publication that provides an emerging view of science, ahead of formal peer review. As we peer over the fence to 2023, here is what my team and I see coming:
Prediction #1: We will enter the ‘prove it’ era in digital health.
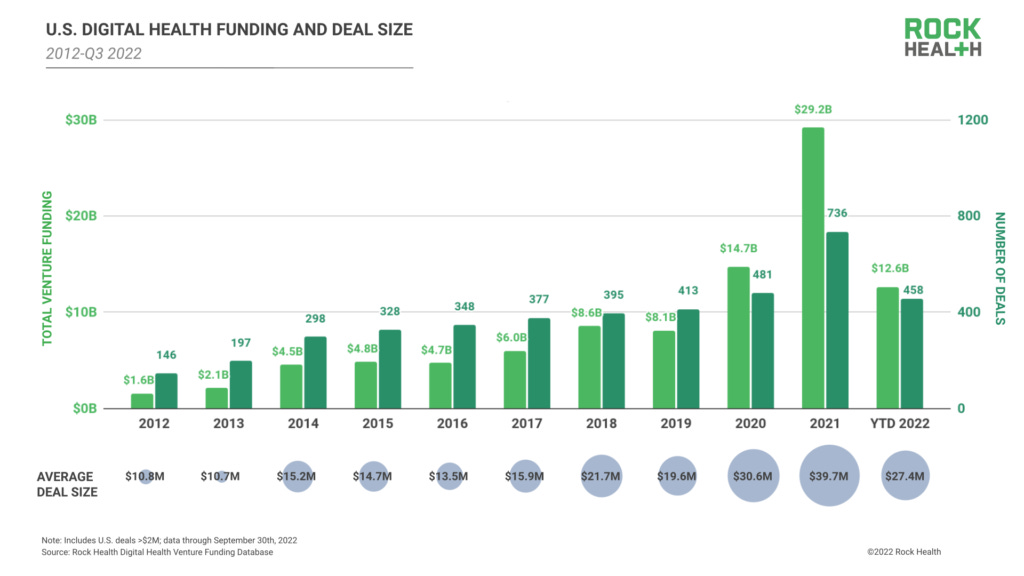
COVID-19 exacerbated frustration with brick-and-mortar healthcare while making healthcare through a screen commonplace. Digital health investment doubled from $14.9 billion in 2020 to $29.1 billion in 2021. The potential was clear. But in 2022 the appetite for hype dissipated. The first wave of digital health companies to go public struggled and private investment shriveled: just $2.2 billion was raised across the sector in the most recent quarter, against the backdrop of rising interest rates and stubborn inflation.
The question many industry participants are asking now is whether 2021 or 2022 is more emblematic of digital health’s long-term promise.
The answer, of course, is neither. Those were the old days of a young industry. Going forward, digital health companies, especially those that sell to employers and insurers, will need credible, third-party validation of ROI, both from improving clinical outcomes as well as increasing business performance. This drive will put even greater pressure on point solutions that focus narrowly on single conditions. Even in rapidly growing spaces like fertility, the value will not come from optimizing the IVF clinic — it will come from ensuring people have the shortest path to bringing home a healthy baby.
This shift is exciting. It suggests that digital health is well-positioned to disrupt the behemoth of our industry.
Prediction #2: Reproductive health will get worse before it gets better — but widespread recognition of the gaps from business leaders will help galvanize change.
Rates of maternal mortality have been rising for decades but the last few years have been particularly gutting. Today, a pregnant woman is 50 percent more likely to die in childbirth than her own mother was a generation ago. Black women in the US are 2-3 times more likely to die than white women, irrespective of education attainment or socioeconomic status, and the pandemic accelerated the crisis. In data released earlier this year, overall maternal mortality increased by almost 20 percent. Nearly all of it was attributable to worsening outcomes for people of color — for Black women the increase was 40 percent; for Hispanic women it was 74 percent.
Then, in June, the Supreme Court overturned Roe vs. Wade.
The decision severely curtailed access to guideline-recommended abortion care, tripling travel times for those seeking abortion while setting in motion a migration of the birth workforce from already underserved parts of the country. There remains unconscionable ambiguity in the delivery room for providers seeking to support patients with high-risk pregnancies.
Early predictions that simply modeled what would happen if more pregnant people were forced to carry pregnancies to term found upwards of a 20 percent increase in maternal mortality was possible. While I am hopeful the situation will not be so dire, and have been encouraged by the response of voters in states ranging from Kansas to Michigan to California to protect access to full-spectrum reproductive healthcare, we are nonetheless entering a dangerous new era for maternal health in America.
Expect corporate America to play an increasingly significant role in helping to turn the tide. Employers are sensitive to ‘bottom-up’ campaigns from employees seeking more and better support, particularly those that test the strength of an organization’s stated commitment to equity. A survey from LeanIn found that 76 percent of women and 74 percent of men under 40 want to work for companies that support abortion access, and an October report from Catalyst shows that support in maternal and reproductive health is viewed as especially essential.
Prediction #3: Mental health and reproductive health will remain essential benefits even amid cutbacks in other categories.
Despite strained wellness and healthcare budgets, don’t expect mental health and fertility, two categories that have exploded in the past few years, to be any less active. First-moving employers that have these solutions in place are already realizing value to their bottom lines. Lagging employers will find them essential to recruiting and retaining a strong workforce.
An emerging trend will also be seen at the intersection of mental health and reproductive health. The traditional approach to supporting fertility patients often overlooks how devastating trying-to-conceive journeys can be on both individuals and couples, who may suffer from feelings of stigma, depression, anxiety, and social isolation and find their clinic ill-equipped to offer support. And following the CDC’s finding that 23 percent of preventable maternal mortality is attributable to mental health conditions, including suicide, there will be greater focus from both the public and private sectors on finding solutions that make mental health a core part of the care model for the full-spectrum of reproductive health. For the people in the back: mental health is health. Here’s to this mantra finally taking root in 2023.
What my team is reading, considering, and building against
Lest I bury the lede, the global population of men is not becoming infertile! In a future Preprint we’ll dive deeper into what we understand about male-factor infertility. For now, let’s just dismantle a recent study in Human Reproduction Update that caused a media sensation by claiming that sperm counts have declined globally by upwards of 50 percent in the last 50 years.
This paper is an update to one the authors published 5 years ago which also caused a sensation. Both rely on limited data and flawed logic. Sperm counts are not tracked systematically. The original study used datasets where men’s age was often unknown. Standardized methodology for counting sperm was not agreed upon until the 1980s. Sperm count in itself is an unreliable measure for determining male fertility. This rebuttal from a year ago can hopefully help many men take a deep breath.
An investigation into the demographics of COVID-19 vaccine clinical trial participants found that women were underrepresented when compared to their percentage of the general population. The consequences were deadly as pregnant women remain the least vaccinated demographic despite being at significantly elevated risk. As I told the New York Times, the fact that only 15 percent of pregnant women have gotten a booster is the direct result of our failure to center this vulnerable population in our public health messaging.
Racial inequity in childbirth is not a uniquely American issue. A new report spearheaded by the NHS in the UK identifies gaps across the system in addressing maternal health disparities. A Black woman in the UK is 3-4 times as likely as a white woman to die from a childbirth-related cause. As in the US, this disturbing status quo is the result of a confluence of factors, including implicit bias in the healthcare workforce. What is unique of course is the country’s nationalized healthcare approach, which makes it all the more striking that the authors call for a ‘national approach’ to addressing these inequities and driving progress.
The journalist Jessica Grose has long taken a widely resonant and clear-eyed look at what it means to be a mother and a parent in America today. Her new book, Screaming on the Inside: The Unsustainability of American Motherhood, is a call to action for compassionate, data-informed policymaking and, more broadly, an empathetic, affirming parenting culture.



Thank you for this insightful read.